What to Know About Gut Microbiome Testing: 7 Things to Expect (And What to Do Next)
Key Takeaways:
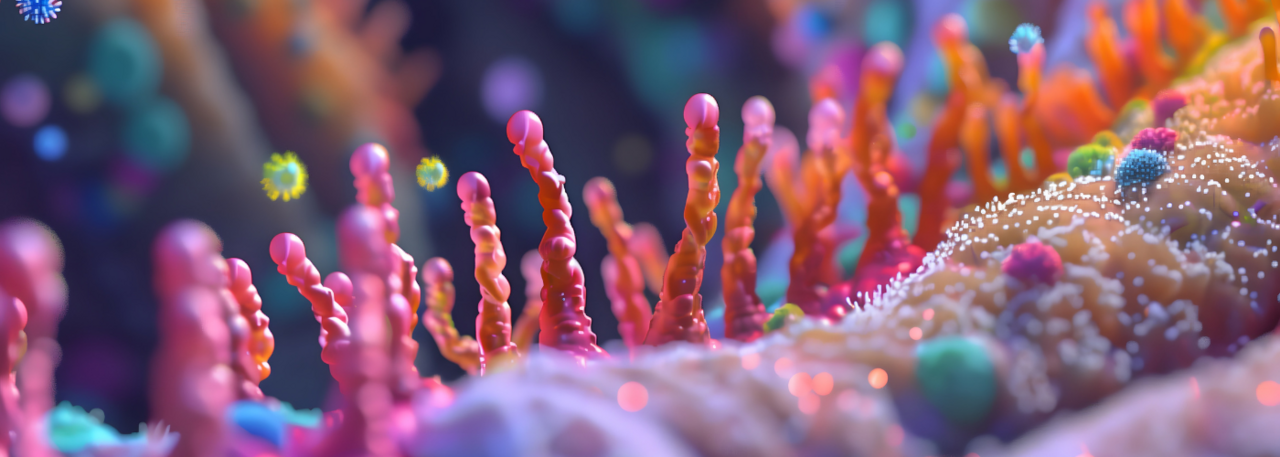
Your gut microbiome is one of the most powerful ecosystems in your body — influencing digestion, immunity, mood, metabolism, and even brain health. So it makes sense that gut microbiome testing has become a recent trend. But if you're thinking about testing your gut microbiome, it helps to know what you're really getting (and not getting) from those results. Gut testing can offer valuable insights — but the test alone won't heal your gut. True gut health starts with rebuilding the gut lining and supporting your gut's foundational health.
Table of Contents:
What Is Gut Microbiome Testing?
Gut microbiome testing analyzes the bacteria, fungi, viruses, and other microorganisms living in your digestive tract — primarily through a stool sample. By looking closely at the makeup of your gut microbiome, these tests aim to provide a clearer picture of what's happening inside your digestive system and how that might impact your overall health.
Depending on the test, results might include information like:
- The diversity of your gut bacteria (how many different species are present)
- Presence of specific pathogens, parasites, or bacterial overgrowths
- Inflammatory markers that signal gut irritation or damage
- Digestive function markers, such as short-chain fatty acid (SCFA) production levels
- Personalized diet or supplement recommendations based on your microbial profile
Some at-home tests go even further, offering insights about food sensitivities, how well your gut microbes break down certain foods, or even how your microbiome might influence things like energy production or mood.
But while these tests can be incredibly informative, it's important to remember that they capture a snapshot of your gut health and don't always tell the full story.
7 Things to Expect from Gut Microbiome Testing
Gut microbiome tests are powerful tools to help you better understand your digestive health, but they can come with a few surprises if you're not sure what to expect. Whether you're taking the test out of curiosity, in response to ongoing symptoms, or as part of a larger health journey, it's important to go in with realistic expectations. Not every result will be black and white, and not all data is immediately actionable without context. Still, these tests can be incredibly helpful alongside thoughtful steps to support your gut.
Here's what you should know before diving into the results:
1. Testing Offers a Snapshot
Microbiome testing captures a moment in time. Your gut bacteria shift based on what you eat, your stress levels, medications, sleep, and more. So, while your results may show helpful patterns, they aren't a final diagnosis.
2. Testing Your Gut Microbiome May Reveal Low or High Diversity Scores
Some tests will give you a diversity score, which reflects how many different types of microbes live in your gut. While more diversity is generally better, low scores aren't always bad news, they just suggest your gut might need more fiber variety or nutritional support.
3. Gut Microbiome Tests Can Flag Pathogens or Bacterial Overgrowth
If you're struggling with gut health symptoms, these tests can help pinpoint imbalances like candida overgrowth or bacterial infections. But context is everything, not all flagged organisms are harmful in small amounts, and interpretation matters.
4. Test Results Can Be Complex to Interpret
Many test results come with scientific language or complex charts. If you're not working with a practitioner, it can be tough to know what to do next. Some companies use algorithms to translate your microbiome data into diet or supplement suggestions based on comparisons to large databases of other test results. While this approach can offer helpful starting points, it's not a substitute for personalized care, and recommendations may feel generic or disconnected from your actual symptoms or history.
5. Gut Microbiome Testing Often Includes Dietary Recommendations
Based on your microbial makeup, you might be given a few food lists to follow — what to eat more of, and what to avoid. This guidance is typically generated by analyzing how certain microbes interact with specific foods or nutrients. It can give you a helpful framework for building gut-friendly meals, introducing more variety, or avoiding ingredients that could be contributing to symptoms.
However, these suggestions are meant to provide general direction, they aren't personalized medical advice. Your overall health history, symptoms, and lifestyle habits still play a crucial role in creating a plan that works best for your body.
6. Your Gut Microbiome Is Always Changing
Your gut microbiome is constantly adapting to your environment, diet, stress levels, and lifestyle choices. What shows up in a test today may look entirely different just a few months later. That means your daily habits play a powerful role in shaping your gut health and you have more control than you might realize.
7. Gut Healing Requires More Than Microbiome Testing
Gut microbiome testing can show you what's going on inside your gut, but results alone won't spark real change. True healing requires more than testing and only happens when you take intentional steps to repair, strengthen, and support your gut lining. Think of testing as a starting point, not a solution. What matters most is what you do after you test.
Testing Is Just the First Step in Healing Your Gut
Testing may help indicate what's going on inside your gut. But testing alone won't rebuild your gut lining, calm inflammation, or restore microbiome resilience. This is where many people get stuck — they see their results, start taking probiotics or antimicrobials right away, and wonder why they're still struggling with symptoms months later.
The reality is that if your gut lining is inflamed, irritated, or compromised, even the best gut health supplements or dietary changes might not deliver results until that barrier is healed. The gut lining acts like a security gate: it decides what gets into your bloodstream and what stays out. When that gate is damaged, it can lead to increased gut permeability (sometimes called "leaky gut"), allowing unwanted particles into the bloodstream and triggering inflammation.
When this happens, you may experience symptoms like:
- Bloating or cramping
- Food sensitivities
- Skin issues
- Brain fog
- Fatigue
- Irregular digestion
That's why supporting the gut lining is the first step to making any gut protocol more effective. One of the most important compounds for gut lining health is butyrate — a short-chain fatty acid naturally produced by certain gut bacteria when they break down fiber. However, many people today struggle to produce enough butyrate naturally. Butyrate acts as the primary fuel source for the cells lining your colon, helping to strengthen the gut barrier, reduce inflammation, and promote overall digestive health. In fact, supporting your gut lining with butyrate can have many benefits, including complementing other common gut health strategies, like probiotics or antimicrobial treatments, by helping create a healthier environment where those interventions can work more effectively.
How to Support Your Gut
Whether or not you decide to test your gut microbiome, you don't have to wait for lab results to start supporting your gut health. Testing can certainly offer helpful insights, but the core foundations of gut healing apply either way. And if you do choose to test, taking action afterward is where the real progress happens.
Supporting your gut starts with repairing the gut lining — but it doesn't end there. Creating a healthy, balanced gut environment means nourishing beneficial bacteria, managing inflammation, and giving your gut the tools it needs to thrive long-term. Think of gut healing as a two-part strategy: reinforce the lining, then nurture the ecosystem within.
Here are key strategies to support foundational gut health:
|
Strategies |
Why It Matters |
|
Butyrate is a short-chain fatty acid that fuels colon cells, supports a strong gut lining, and promotes microbial balance.* |
|
|
Diverse, Fiber-rich Foods |
Different bacteria feed on different fibers. Variety helps grow a resilient microbiome. |
|
Certain foods — like fermented vegetables, artichokes, garlic, and flaxseeds — help feed beneficial microbes and support short-chain fatty acid production, which improves gut barrier function and microbial balance. |
|
|
Stress Management |
Chronic stress disrupts the gut-brain axis and impairs digestion. |
|
Avoid unnecessary antibiotics or NSAIDS |
These can harm beneficial bacteria and thin the gut lining. |
|
Focus on anti-inflammatory support |
Nutrients like glutamine, omega-3s, and collagen help soothe the gut. |
Gut Health Isn't Just About Testing, It's About Taking Action
Gut microbiome testing can offer valuable insight into what's happening inside your gut — from the types of microbes living there to potential imbalances or patterns worth exploring. But testing alone won't create lasting change (and it's not required when working on your gut health).
Regardless of test results, building a strong foundation is the first step on your gut health journey. That means repairing and supporting your gut lining, nourishing beneficial bacteria, and creating an environment where your microbiome can thrive. Testing can guide your strategy, but consistent action is what turns information into real transformation.